Antibiotics are a staple of modern medicine and save millions of lives every year. But they can be harming the normal bacterial system our health relies on.
Our bodies host trillions of bacteria that we can't live without – with the highest density in our guts. But are we permanently damaging this crucial part of our body every time we take antibiotics?
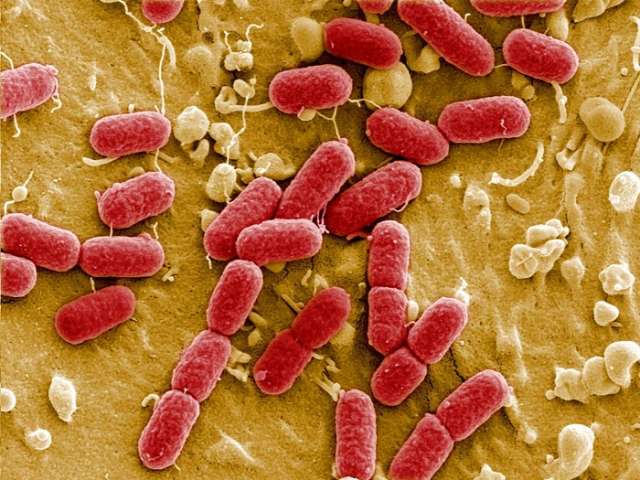
"The gut microbiome is a complex network of microbiotic lifeforms and all the things they need to sustain themselves in the niche of the body," says James Kinross, a consultant colorectal surgeon at Imperial College London.
The gut microbiome plays a huge role in maintaining our health, including regulating the immune system and aiding digestion. And experts argue that antibiotics are one of the biggest threats to our gut microbiomes.
Antibiotics, commonly prescribed to treat and prevent bacterial infections, are a cornerstone of modern medicine. But in the process of targeting the infection-causing bacteria in our bodies, antibiotics can also inadvertently wipe out the other bacteria in our bodies.
There are growing concerns among scientists about the health implications of our increasing reliance on antibiotics; between 2000 and 2015, global prescriptions of antibiotics increased by 65%. The problem with this rising use of antibiotics is two-fold: the damage caused to our gut microbiomes, and growing bacterial resistance towards antibiotics.
Antibiotics have become a cornerstone of modern medicine, but there are increasing concerns around overuse (Credit: Getty Images)
"Antibiotics disrupt the intricate ecosystem of our gut microbiome, and, in doing so, put the surviving bacteria at greater risk of donating their resistant genes over to pathogens," says Gautam Dantas, professor of laboratory and genomic medicine at Washington University's School of Medicine in St Louis in the US.
We know that the more diverse our gut bacteria population is, the better. But every course of antibiotics disrupts this population because antibiotics aren't targeted enough to only kill the pathogenic bacteria causing the infection. Instead, they go after all bacteria in our guts.
"There's collateral impact," says Dantas. "Think of a forest where you're trying to get rid of one weed infection; the way we deploy antibiotics is to carpet-bomb the forest, killing the good and the bad."
When scientists have looked retrospectively at the microbiomes of people who have had an infection followed by a course of antibiotics, they've found that microbiome diversity largely recovers within a few months, Dantas says. But in some people, some good bacteria never show up again, he adds.
Dantas and his team of researchers have studied faecal samples collected from children treated at the paediatric hospital connected to his laboratory. These samples were collected routinely, before any infections and antibiotics, which allowed his team to see the changes in children who get an infection and are given antibiotics later on.
Dantas has used these samples to compare changes to the gut microbiome after antibiotics in two groups of infants – pre-term babies, who are born before 36 weeks, and term infants, born after 36 weeks.
"What we know happens in adults after antibiotics happens more dramatically in babies: a lower diversity of the microbiome, and huge spikes in drug-resistant genes," he says.
While the effects differ from person to person, and depend on our age, the consensus among scientists is that the effects of one course of antibiotics can be permanent.
"Some people are very susceptible to damage in [their] microbiome from antibiotics, and their ecology of their microbiome will change dramatically and never return to what it was before the antibiotic dose," Kinross says.
"We're losing diversity in our guts and crucial microbes that have sustained us for hundreds of thousands of years [are being lost] on an unprecedented time scale."
But scientists are still trying to work out the long-term health consequences of antibiotic use on our gut microbiomes.
"We know that antibiotics have the capacity to affect every single domain of microbiome function." Kinross says. "They don't just lead to a depletion in the number of bacteria, but they also effect the function of microbes in complex, individualised ways that we don't understand well."
It's not just the impact on the gut bacteria that is causing concern, but also secondary consequences on the development of the immune system, Kinross adds.
Studies show that taking recurrent doses of antibiotics has a cumulative effect, and the impact is also greater if you take a take a more broad-spectrum dose. This is often referred to as the "multiple hit hypothesis".
"Those random extension events, every now and again, will hit a critical bug," says Dantas. "This is the weird evolutionary experiment we're running on ourselves every time we take an antibiotic."
The other consequence of long-term antibiotic use is the risk of resistance. When a population of bacteria is exposed to an antibiotic, those that lack the genes for antibiotic resistance tend to die off. But ones which do have them – either genes they have picked up from their environment, or mutations that have arisen spontaneously – will survive. In this way, the drugs actively select for bugs that are antibiotic-resistant. This becomes a problem when pathogenic bacteria reap the rewards of this adaptation.
"Every time we deploy antibiotics, it increases the proportional risk of the gut microbiome being enriched for drug-resistant genes, so that next time the pathogen comes around, it might be able to pick up some of these selective resistant genes from the gut," Dantas says.
And this process isn't confined to our guts, says Craig MacLean, professor of evolution and microbiology at the University of Oxford. "Resistant bacteria can migrate from the gut to other areas, so what happens in the gut has an impact on the rest of our body," he says.
The harmful and life-saving impact of antibiotics is one of the biggest conundrums troubling scientists around the world. While there is no one solution, there are approaches which could mitigate the harmful effects of antibiotics on our health.
"Antibiotics are amazing medicines that have saved millions of lives. They're very precious resources and should be used, but we need to understand how to precisely target them," says Kinross.
Scientists are now looking at antibiotics that are more targeted towards parts of the body, as well as ones that target specific bacteria, MacLean says, with the idea of only getting rid of the bacteria you want to get rid of, and leaving beneficial bacteria in the gut intact.
But the biggest tool currently at our disposal, says Anthony Buckley, associate professor in gut microbiology at the University of Leeds, is our diets. "Nutrition is one of the biggest drivers behind establishing the human microbiome," he says.
The University of Leeds' healthcare associated infections research group has been testing the effects of antibiotics on the microbiome for the last two decades.
The highest variety of foods we eat is usually associated with a higher variety of microbes in the gut, and fibre in particular seems to have a really positive impact," says Ines Moura, a research fellow at Leeds University's faculty of medicine and health, who is currently testing the effects of different nutrients on the gut microbiome and how they can reduce the negative effects of antibiotics.
Dietary fibre is particularly important because microbes in our body digest it and produce short chain fatty acids, which provide energy to the cells lining the colon, says Buckley.
"When you have antibiotics, the microbes that produce short-chain fatty acids get depleted and take time to recover. Our theory is that, by ingesting dietary fibre, they're providing a substrate for those microbes to grow on and produce short-chain fatty acids, and hopefully establish balance again," he says.
The irony underlying the use of antibiotics is that, with each course we take, we potentially lower our body's ability to fight infection, and, therefore, increase our reliance on antibiotics.
"It's much better to not have to rely on antibiotics," Kinross says, "And instead focus on the bio-resilience of our internal ecology by eating healthily, particularly in a person's early life, since this is when antibiotics cause the most damage."
More about: