Pricey Hepatitis C drugs can have deadly side-effect for some
Doctors who prescribe any drug for hepatitis C patients need to screen them for hepatitis B as well, the FDA said.
"Doctors should be screening everybody," said Dr. John Farley, deputy director of FDA`s Office of Antimicrobial Products.
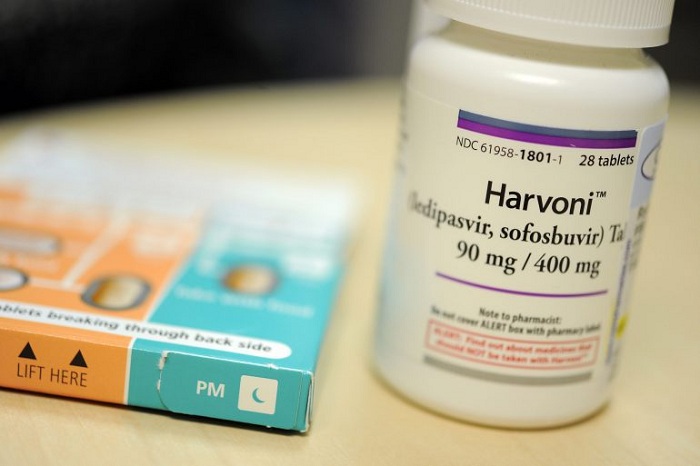
The drugs are called direct-acting antivirals, and they include Sovaldi, knowns generically as sofosbuvir; Harvoni, a combination pill that includes Sovaldi; Olysio or simeprevir; Daklinza or daclatasvir; Technivie and several others.
"We identified 24 cases of hepatitis B reactivation reported to FDA and from the published literature in hepatitis B/ hepatitis C co-infected patients treated with direct-acting antivirals during the 31 months from November 22, 2013 to July 18, 2016," the FDA said in a statement.
"This number includes only cases submitted to FDA, so there are likely additional cases about which we are unaware. Of the cases reported, two patients died and one required a liver transplant," it added.
"As a result, we are requiring a Boxed Warning, our most prominent warning, about the risk of hepatitis B reactivation to be added to the drug labels of these direct-acting antivirals."
Hepatitis C affects about 3.2 million Americans, once killing more than 15,000 each year, mostly from illnesses such as cirrhosis and liver cancer.
The new drugs have changed that — at a steep price.
Gilead`s Sovaldi costs about $84,000 for a weeks-long regimen that can cure someone of hepatitis. The second-generation version, called Harvoni, costs more than $94,000 for similar treatment.
About 5 percent of veterans have hepatitis C — five time the rate of the rest of the U.S. population, according to the Department of Veterans Affairs.
It`s not known how many people also have hepatitis B, but the risk factors are similar: sex, intravenous drug use, and other contact involving blood. About 1 million Americans have hepatitis B, and 3,000 a year die of it.
Both viruses affect the liver and can often cause considerable damage before people develop symptoms.
Only half of people in the United States who have ever been infected with hepatitis C get proper testing for it. And people may not remember they have also had hepatitis B, which has no cure but which can go dormant.
"Health care professionals should screen all patients for evidence of current or prior HBV infection before starting treatment with direct-acting antivirals, and monitor patients using blood tests for hepatitis B flare-ups or reactivation during treatment and post-treatment follow-up," the FDA said.
There are drugs to treat hepatitis B, but they don`t cure it.
Farley said the FDA noticed some reports of hepatitis B reactivation in people taking the hepatitis C drugs about a year ago. It`s taken months to gather more information, he said.
Now that the risk is clear, the FDA wants to issue the strongest possible warning, he said. Specialist liver disease experts will likely screen for hepatitis B but many non-specialists may not realize the need, he said.
"You just don`t want to figure it out late," he said.
It`s still not clear why treating hepatitis C would affect a dormant virus like hepatitis B, Farley said.
"The mechanism of action is not clearly understood," he said.
"I think it is important to recognize that these hepatitis C drugs are lifesaving medications. What we don`t want to do is discourage patients with hepatitis C from getting treatment," he told NBC News.












































