In Embryo Research We Need Laws First, Then Science
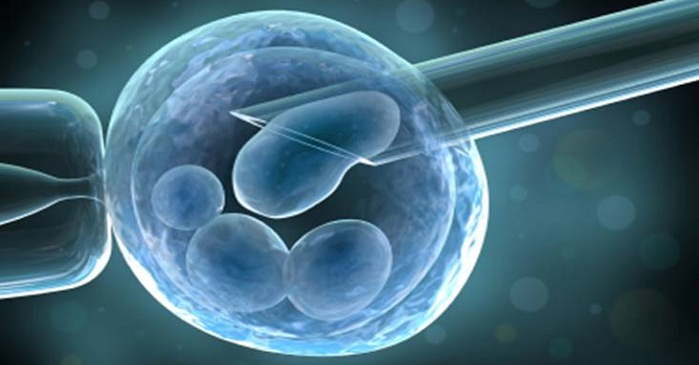
The British researchers will try to better understand the genes that produce miscarriages, which may lead to improved fertility treatments. This study is also set up to avoid a common concern raised about germ line alterations: the unknown consequences of allowing changes to the human genetic code that can be passed on to future generations. Because the researchers will not transfer the embryo in a mother or allow it to develop past 14 days, the study avoids the issue of how changes made through CRISPR may affect a living child down the road.
This study has the potential to significantly contribute to scientific understanding, while avoiding some concerns about the possible harms of using CRISPR, and thus its approval makes sense as long as there is adequate consent of the embryo donors and the embryos are not created for research purposes.
Yet a primary concern remains regarding what this project’s approval means in terms of the speed and direction of the field of gene-editing technology. Is this approval another significant step towards a world of “designer babies” and changes to DNA that will be passed down to future generations? While this particular study may pass ethical scrutiny, how do we make sure further projects don’t take us too far down this road?
While some may want to ban the use of CRISPR on human embryos, that approach is unlikely to be generally supported, in large part because of the significant benefits gene-editing may yield, both in understanding human genes and in allowing new approaches for treating health problems. Thus one central concern, as researchers propose more possible applications of gene-editing, is making sure this research progresses safely. It is therefore crucial to give attention to how CRISPR research and possible eventual treatments are being regulated.
The U.K. has a robust system for regulating human embryo research, as well as in vitro fertilization, through the HFEA. Ethical concerns raised by subsequent projects will be reviewed and assessed by the HFEA. In contrast, the U.S. has sometimes been referred to as a “Wild West” of reproductive technology. The National Institutes of Health has a number of restrictions on what can be funded. In contrast, privately funded gene-editing projects are not regulated by a central agency or framework that can address concerns of safety and efficacy, or balance the interests of research with the protection of patients.
Given the relative ease and inexpensiveness of CRISPR technology, the raises the possibility of U.S. IVF clinics jumping prematurely into trying to use CRISPR for reproduction. Preliminary findings coming out of the U.K. could inspire someone in the U.S. to try to offer reproductive treatments, long before the technology is proven safe and effective. More broadly, the lack of regulation could mean that instead of research that builds incrementally upon previous research, we may be left with a situation where purported therapies that are not ready for mass adoption can proliferate.















































