Lung cancer drug may be early clue in the hunt for an HIV cure
The drug, nivolumab, is used in treating advanced cancers and appears to be able to target the “latent reservoirs” of HIV-infected cells that prevent the virus being wiped out, requiring life-long treatment.
The authors acknowledge that this is just one example from a trial in 50 patients, one of whom showed no improvements, and further clinical trials are needed.
But the study’s lead, Professor Jean-Philippe Spano, head of the medical oncology at Pitié-Salpêtrière Hospital in Paris, France said it was the first demonstration of a theory that nivolumab could target HIV this way.
“It was thought, but until now not demonstrated, that inhibitors of immune check-points [like nivolumab] could, in a similar way, wake up dormant HIV-infected cells and also the immune defences against the virus,” he said.
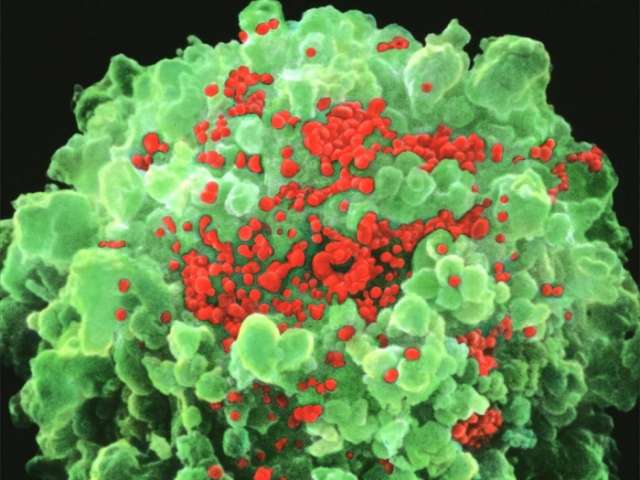
HIV infects the white blood cells that make up the body’s immune response, reducing their ability to fight off infection.
Anti-retroviral drugs used in treating HIV prevent the virus from replicating but aren’t able to tackle these dormant reservoirs of infected white blood cells in bone marrow, and the brain.
Professor Spano said these dormant cells are infected but “are not actively producing HIV” and aren’t visible to the weakened immune system.
These reservoirs “are established during the earliest stage of HIV infection” and when treatment is stopped they can reactivate and begin producing the virus again.
Nivolumab was theorised to remove a cellular brake that is preventing virus production and kick start the immune system to tackle infected cells.
While no HIV was detectable in this patient’s blood prior to starting nivolumab, virus levels began to increase after treatment along with the activation of infected cell killing “T-cells”.
Professor Spano said: “In this patient we observed, as expected, both a re-activation of HIV and an increase in CD8 T-cell responses against HIV, which resulted in the drastic decrease in the HIV reservoir, thus leading to a sustained reduction of the HIV reservoirs.
“This is the first demonstration of this mechanism working in humans. It could have implications for HIV patients, both with and without cancer, as it can work on HIV reservoirs and tumour cells independently.
The letter says it remains to be seen if the results can be repeated, but adds: “This first report of a successful depletion of the HIV reservoirs opens new therapeutic perspectives towards an HIV cure.”
Scientists unrelated to this study also said caution was needed in interpreting this single case.
Professor Stephen Evans, professor of pharmacoepidemiology at London School of Hygiene and Tropical Medicine, said the findings show a large effect, but larger trials are needed.
“Until we have such data talks of ‘cure’ are premature, but it could lead to new approaches in dealing with HIV.”
Dr Andrew Freedman, a reader in infectious diseases and an honorary consultant physician at Cardiff University, said this case showed an “impressive reduction” of the latent HIV reservoir, which is the reason patients currently need lifelong treatment.
He said larger studies would show if the treatment was safe and effective enough to be used more widely in HIV patients without cancer, and whether the reservoir would come back.
“Nevertheless, this is a potentially exciting finding and it is possible that nivolumab, most likely in combination with other approaches such as therapeutic vaccines, may have a role in the eventual discovery of a cure for HIV.”















































