Blood-clotting drugs, normally used to tackle minor bleeding rather than as cancer treatment, were carried by nanobots, made from origami-folded DNA sheets, to shut off the blood supply to tumours throughout the body.
Starved of their blood supply, tumours began to shrink and the cancer’s ability to spread and grow in new sites also appeared to be reduced, doubling the life expectancy or removing tumours entirely in some mouse cancers.
This demonstration, which marks a major step towards the implementation of nanobot drug delivery in medicine, could pave the way for delivering toxic chemotherapy drugs with reduced side effects, among a host of other uses.
“We have developed the first fully autonomous, DNA robotic system for a very precise drug design and targeted cancer therapy,” said Professor Hao Yan, director of the Arizona State University Biodesign Institute’s Centre for Molecular Design and Biomimetics.
“Moreover, this technology is a strategy that can be used for many types of cancer, since all solid tumour-feeding blood vessels are essentially the same,” he added.
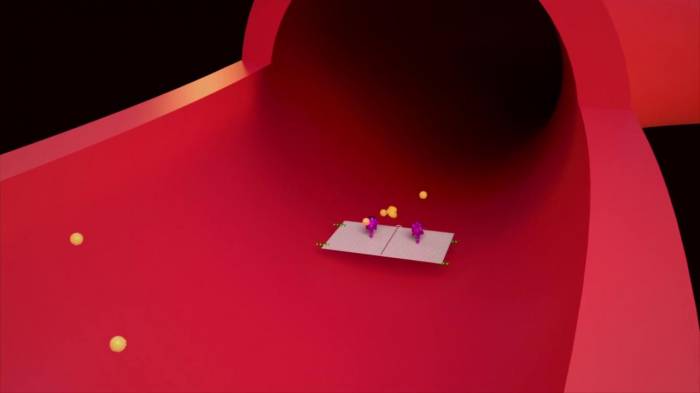
These nano-machines are not miniaturised metal craft, as in science fiction, but instead use DNA fragments as a building block, precisely folded to fit its purpose.
In this case fragments of DNA are arrayed in sheets that can be zipped up to encase a drug payload, preventing it interacting with healthy cells and stopping short-lived drugs being broken down.
They also require a release trigger, a molecule which will only respond to a chemical signature on the outside of cancer cells, which unzips the nanobot exposing the treatment.
In this study, published in the journal Nature Biotechnology today, the DNA sheets were folded into a tube shape to encase blood-clotting drug, Thrombin.
The drug is used to treat bleeds after surgery but breaks down quickly to target tumours.
The international team, including researchers from China, Australia and the US, primed their nanobots to release in the presence of the protein molecule, nucleolin, which coats the internal walls of blood vessels feeding tumours.
Within 24 hours of the treatment the scientists saw blood vessels feeding the primary tumour site had been cut off, with solid clots forming in all tumour blood vessels over the next 72 hours – causing the tumour to start to die.
The treatment was most effective in treating mice with melanoma cancers, which have a very strong blood supply, where three out of the eight mice treated showed complete regression of their tumours.
Life expectancy in treated mice was 45 days, compared to 20.5 days in non-treated mice.
However, the team showed nanobots were also able to home in on breast cancers and shrank or reduced the size of less vascularised ovarian cancer tumours, and lung cancers.
Crucially, no clots were formed away from tumour sites, or in key organs in the heart, liver, lungs or kidney, verifying that the treatment was only targeting cancer cells.
They also showed the system works safely in larger animals, Bama miniature pigs, which have “high similarity to humans in anatomy and physiology”.
“I think we are much closer to real, practical medical applications of the technology,” said Professor Yan.
“Combinations of different rationally designed nanorobots carrying various agents may help to accomplish the ultimate goal of cancer research: the eradication of solid tumours and vascularized metastases”.
The nanobots could also be used in non-cancer treatment to target drugs to diseased organs or infections.
Independent academics said the animal test results could have promising implications for humans.
Professor Peter Dobson of the Queen’s College, University of Oxford, said: “It is a neat idea and there is a lot of evidence in the paper to show that this is a promising approach. It should be said that it has only been done so far in animals.”
While Professor Dorothy Bennett, director of the Molecular and Clinical Sciences Research Institute at St George’s, University of London, agreed, she noted that the target of new blood vessels might limit its use in some cases – should it be shown to work in human cancers.
“This could potentially have a therapeutic effect in adults with cancer, where generally there will not be any newly forming blood vessels except within the growing cancer,” she said.
“It would not presumably be specific enough if there were any other growing blood vessels present, for example in growing infants or in people with healing wounds.”
























-1745485667.jpg&h=190&w=280&zc=1&q=100)





















