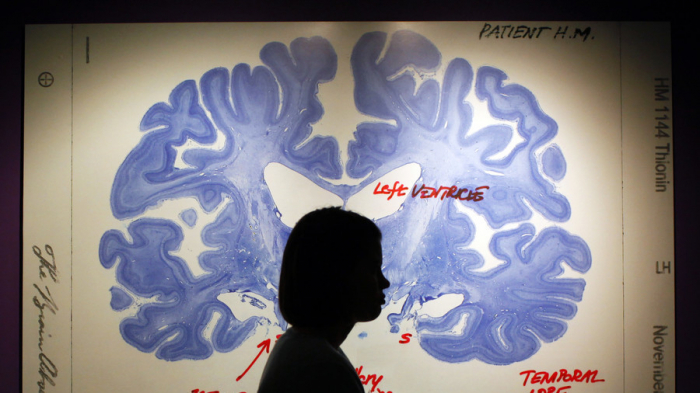
Increasingly common but still poorly understood, depression is a modern mental health plague, affecting 300 million people worldwide every year. Scientists at the University of California at San Francisco believe they’ve found a new way of treating the condition using deep-brain stimulation (DBS). Currently used to treat Parkinson’s and epilepsy, DBS involves implanting electrodes into specific areas of the brain and delivering controlled doses of electricity through a pacemaker-like device. The impulses are thought to restore a healthy electrical pattern, alleviating the patient’s symptoms.
Previous attempts at using DBS to treat depression had mixed results, sometimes catapulting depressed patients into mania or even making them more depressed, but the UC team zeroed in on the orbitofrontal cortex (OFC) – uncharted neurological territory that appeared advantageous both for its role in emotion processing and its plentiful connections to other parts of the brain involved in emotional regulation.
Given access to a small group of epileptics who already had electrodes implanted into various parts of their brains to pinpoint seizure locations – a hyper-specialized population that means their results are unlikely to be replicated anytime soon – the researchers stimulated different brain regions over a period of several days, sometimes swapping in a “sham stimulation” to act as a control.
Afterwards, subjects were asked about their mood. Depressed subjects were consistently happier following OFC stimulation in a way non-depressed subjects were not, and the effect did not appear following sham stimulation. Unlike in previous DBS experiments, the positive mood appeared natural – both in how the subjects behaved and how their brainwaves looked on an EEG.
The results of the study, published in Current Biology, provide a much-needed boost for the ailing DBS-for-depression-treatment paradigm, which suffered a major blow after a large 2013 trial was discontinued for producing poor results. Other trials ended more ambiguously with temporary, erratic improvements, but the results of this experiment have encouraged the team to pursue the OFC further as a stimulation site for depression treatment.
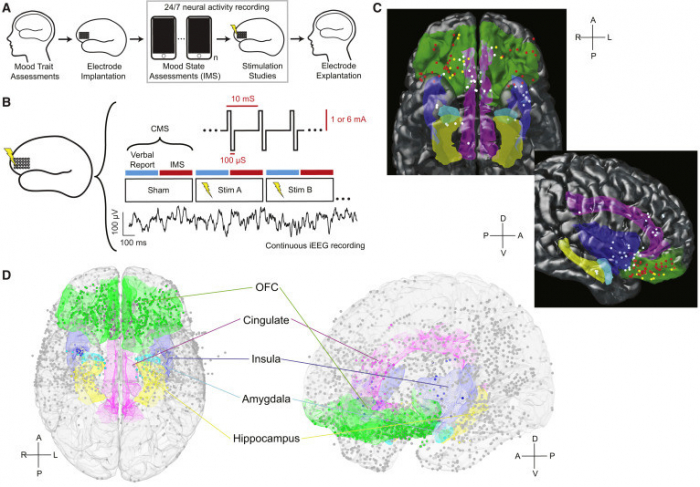
© Current Biology
Depression is notoriously resistant to treatment, and current drug-based therapies fail many patients. Surprisingly little is known about the mental circuitry responsible for depression – the serotonin-imbalance theory has been repeatedly debunked, though effective marketing means 13 percent of Americans continue to take antidepressants devotedly.
The researchers admit little is known about how exactly DBS produces the “complex behavioral changes” seen in their study, but what’s the harm in trying to make the novelty tech more mainstream? Oh, right… Just last month cybersecurity experts warned about the vulnerabilities of neural implant technologies that can potentially expose the human brain, opening an entire new era of brain hacking, identity theft and memory black market.
RT
More about: brain