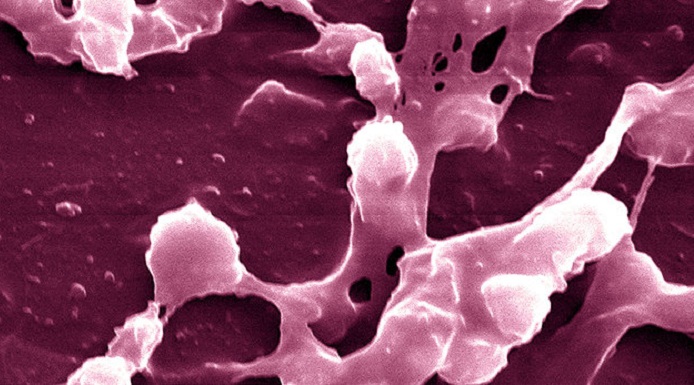
The bacterium Staphylococcus aureus -- known to cause "staph" infections, a type of soft tissue bacterial infection -- is a major public health threat, responsible for a growing number of serious illnesses and deaths.
In its antibiotic-resistant form, Methicillin-resistant Staphylococcus aureus, or MRSA, causes more than 80,000 infections and 11,000 deaths each year. While MRSA is resistant to many antibiotics, it does respond to others, and the infection is often treated with a combination of two or more antibiotics for this reason.
But the study, which appeared in the journal Cell Host & Microbe on Wednesday, finds that one of the most common antibiotics used to treat the infection may inadvertently activate the body`s own pathogen-defense system and worsen MRSA skin infections.
Dr. George Liu, a researcher at Cedars-Sinai Medical Center in Los Angeles and one of the study`s authors, said in a statement individuals infected with MRSA who receive a beta-lactam antibiotic -- a broad class of medicines that includes penicillin derivatives -- "could end up being sicker than if they received no treatment at all."
"Our findings underscore the urgent need to improve awareness of MRSA and rapidly diagnose these infections to avoid prescribing antibiotics that could put patients` lives at risk," he said.
While the staph bacteria is often carried on the skin and in the noses of healthy people, MRSA colonizes roughly 1 percent of people. The typical treatment is beta-lactam. In the study on mice, the researchers tested the immune system`s response to those antibiotics.
The scientists gave a high number of MRSA bacteria to the mice, eliciting an infection. Then, they administered beta lactam antibiotics to treat the infection. That caused the mice to become sicker.
"[In mice], we clearly see that treating the infection with a beta lactam antibiotic makes the infection a lot worse," Liu told The Huffington Post. "How that translates to human infection is less clear."
Normally, staph bacteria uses certain proteins to build its cell wall. Beta-lactam antibiotics kill the bacteria by inhibiting these proteins. The MRSA makes a new version of the protein that is affected somewhat by the antibiotics, and is less effective in building the cell wall than the normal protein. So, MRSA ends up building a weak cell wall. The immune system detects this difference and responds extra-aggressively, attacking the weak cell wall.
"In situations where there is a lot of infection, this highly aggressive response can cause extensive inflammation and tissue damage, effectively making the consequences of the infection worse," Liu said.
This presents a challenge for physicians, as they often turn to beta lactam antibiotics as a first line of defense to treat staph/MRSA infections because they are usually effective. But the findings show that these antibiotics may make the infection worse if it turns out to be MRSA -- which takes doctors a few days to determine.
Trials on humans are needed before researchers can suggest guidelines for correct antibiotic use to treat staph and MRSA.
"In published studies, between 30 to 80 percent of patients who have moderate or severe MRSA infections have been given the wrong antibiotic," Liu said. "Our hope is that by understanding better the pros and cons of picking between the various antibiotics that are available, we can improve patient care."
More about: