T-cell immunotherapy hit headlines last year when British baby Layla Richards became one of the first people in the world to be given the treatment, which is made from the body’s own cells.
Now, two landmark studies have revealed the therapy’s stunning potential.
One suggests it will last for at least 14 years in the body, raising the tantalising prospect of a permanent cure for cancer.
In the other, 94 per cent of terminally ill patients saw the disease vanish completely.
The ‘extraordinary’ results – seen in so-called ‘liquid’ cancers such as leukaemia rather than those that form solid tumours – are ‘unprecedented in medicine’, the world’s biggest science conference heard.
Researcher Chiara Bonini said: ‘This really is a revolution.’
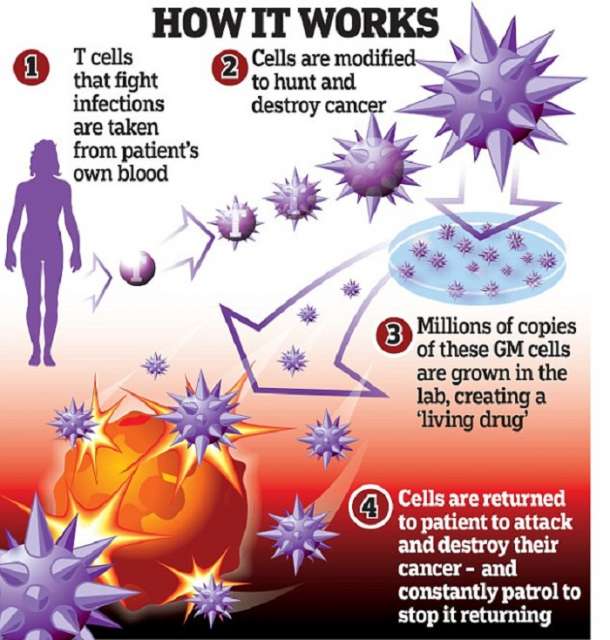
The treatment is created from T-cells – white blood cells that normally fight off viruses and bacteria – which are removed from the patient and genetically tweaked to recognise and attack their cancer.
The genetically-modified cells are then grown in their millions in a lab before being infused back into the patient, where they hunt down and destroy the cancer cells. Scientists around the world are perfecting the technique, and a series of trials have shown it to have remarkable potential.
Some of the most exciting results come from the San Raffaele Scientific Institute in Milan, where doctors gave ten patients infusions of T-cells and watched how long they lasted in the body.
One type of T-cell survived for 14 years, the conference of the American Association for the Advancement of Science heard.
Dr Bonini said these cells may last for life. If they were also genetically engineered to hunt out and destroy cancer, they would patrol the body year after year and stop it from ever returning.
She likened the therapy to a vaccine that gives protection for life against an infection, adding: ‘T-cells are a living drug and they have the potential to persist in our body for our whole lives. Our findings have profound implications for the design of T-cell-based immunotherapies.’
Dr Bonini said patients were ‘very close’ to the first treatments becoming widely available.
Professor Daniel Davis, a Manchester University expert on the immune system, described the study as ‘an important advance’.
He said: ‘The implication is that infusing genetically-modified versions of these particular T-cells could provide a long-lasting immune response. Immunotherapy has great potential to revolutionise cancer treatments and this study shows which type of T-cells might be especially useful to manipulate.’
A second study, also presented at the conference in Washington DC, reinforced the potential of T-cell immunotherapy.
When scientists at the Fred Hutchinson Cancer Research Centre in Seattle gave genetically-modified T-cells to leukaemia patients with months to live, the cancer disappeared in 94 per cent of cases. Patients with other blood cancers saw response rates of greater than 80 per cent, with more than half experiencing complete remission.
Researcher Dr Stanley Riddell said: ‘These are patients that have failed [every other treatment].
‘Most patients in our trial would be projected to have two to five months to live.
`This is extraordinary... unprecedented in medicine to get response rates in this range in these very advanced patients.
‘We have a long way to go. The response is not always durable, some of these patients do relapse … but the early data is unprecedented.’
Professor Dirk Busch, a T-cell researcher at the Technical University of Munich, said: ‘We have now for the first time genetically engineered T-cells in patients.
‘A couple of years ago, nobody would have expected that they would work so nicely, that they would survive so nicely. That opens the door for getting more creative and making better cells.’
The treatment is not without its challenges, including side-effects that can be severe and even fatal. Success so far has been in leukaemia and other ‘liquid’ cancers, rather than prostate, breast and other tumours that form lumps.
Getting T-cells deep inside solid tumours will be difficult. Cost is also an issue, as the treatment is tailored to individual patients.
Cancer Research UK’s Dr Kat Arney said it was an ‘exciting prospect’.
She stressed that it ‘doesn’t yet work for all patients … we still need more results from more trials … but there’s a lot of hope this type of therapy could save lives’.
‘Like a vaccine that protects for life.’