The predictive modelling is published on Friday in Lancet by Université Laval, Harvard University and Cancer Council New South Wales working with the World Health Organisation. All three teams independently developed their models based on the biological understanding of cervical cancer, and multiple data sources from multiple countries located in east Asia and Pacific, Europe and central Asia, Latin America and Caribbean, the Middle East and North Africa, South Asia, and sub-Saharan Africa.
“One of the exciting things for us about the new studies is the three teams did independent work but got very similar results,” director of research at Cancer Council NSW and adjunct professor Karen Canfell said.
While there has been some success in high-income countries like Australia, cervical cancer is still the fourth-most common cancer for women in the world, and the leading cause of cancer death in some low-income countries.
A large majority of the 570,000 new cervical cancer cases worldwide in 2018 were in women living in low- and lower-middle income countries.
The combination of vaccination of girls, along with twice-lifetime cervical cancer screening and access to invasive cervical cancer treatment was predicted to reduce cervical cancer incidence by 97% and mortality by almost 99%, averting more than 74 million cervical cancer cases and more than 62 million deaths in the next 100 years, she said.
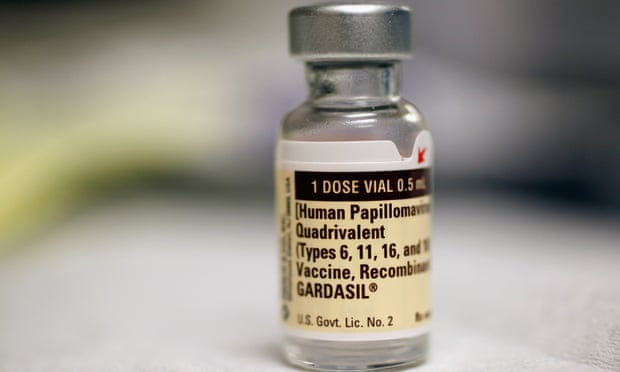
To reach this goal in the 78 low- and lower-middle income countries, the countries will need to get to 90% of girls vaccinated against human papillomavirus (HPV), 70% twice-lifetime cervical screenings with HPV testing, and 90% coverage for treatment of pre-invasive lesions and invasive cancer by 2030.
“The idea is countries will use this to understand the impact of decisions that are made for investing in health today,” Canfell said.
The research will be considered by WHO’s executive board next week, and by countries at the World Health Assembly in May.
Australia has led the charge in preventing and treating cervical cancer, and last year Canfell said Australia was on track to eliminating cervical cancer by 2035, and this week, Public Health England also released a study showing that as of the end of 2018 – 10 years since the vaccination program was introduced – there were no HPV infections detected in 16 to 18-year-old females.
Canfell said every country would have its own challenges in implementing vaccinations, screenings and treatments.
“All three of those interventions are proven, and they’re very effective in high-income countries, but they all have challenges in terms of logistics and implementation,” she said.
“One of the biggest challenges is all three things will have to be country-level considerations of how to do it within the health systems that exist, or building health systems to implement these interventions. There will certainly be differences in the way things are implemented.”
More about: